New advances in medicine and technology have improved health-care for both patients and doctors across the world. Many patients with chronic illness can be treated for diseases instead of symptoms, and new treatment regimens can help people of all ages live healthier lifestyles.
While many of these advances have improved health-care, they also introduce many challenges for doctors and service providers.
The following list portrays some of the greatest challenges faced by doctors as technology and patient care evolves.
1. Self-Diagnosis and Treatment by Patients
With the advent of the Internet, many patients are seeking diagnosis information online. While websites such as Wikipedia and WebMD are valuable, they can be a crutch in communicating health information to patients.
Many patients will self-diagnose online, and begin treatment without the oversight of a doctor. While health information available online is usually accurate, self-diagnosis involves an unprofessional and potentially dangerous interpretation of disease symptoms.
Many patients may not diagnose symptoms of an illness correctly, which can lead to a false diagnosis. This can result in a severe illness being misdiagnosed as a benign disease, and vice versa.
Further complicating the situation, some treatment options may be inappropriate for some patients, and can endanger their health.
2. Conflicting Treatment Plans with Self-educated Patients
Doctor-patient communication becomes impaired when patients self-diagnose. Many patients trust information found online more than that provided by a primary care physician.
Some patients will verify and factcheck all treatment options or diagnoses stated by a healthcare provider, without understanding the full process behind the diagnosis.
This can lead to lapses in treatment, belligerence in communication with healthcare providers, and failure to schedule follow-up visits.
3. Information Overload
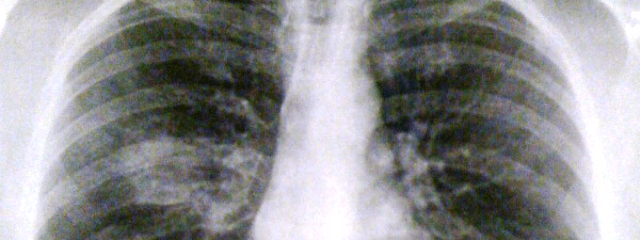
Doctors and other health-care providers have access to a variety of screening and diagnostic tools. The information from these tools can yield large amounts of physiological data, which can become cumbersome and unwieldy to interpret.
A traditional doctor check-up may involve a check of blood pressure, pulse, temperature, appearance, and a physical examination.
New technology can yield much larger sets of data, ranging from a variety of physiological responses to stimuli in the environment, to induction of disease through variable gene expression.
Interpreting large data sets requires the use of novel technology. Many symptoms may not provide adequate information for an individual to interpret, but machine-learning technology can build diagnosis guides using these large data sets.
A wide variety of symptoms may not present any individual disease to a healthcare professional, but a disease that shows all these symptoms can be diagnosed using machine learning technology.
It’s important for doctors and healthcare professionals alike to understand the learning and diagnostic limitations of both humans and machines.
By combining computer-aided diagnosis with the guidance of a healthcare professional, many diseases can be diagnosed before emergent symptoms become a health hazard.
4. Bias in Treatment Options Provided
Many doctors and healthcare professionals are inundated with a barrage of pharmaceutical representatives, medical equipment salespeople, and software service providers.
Many journals of medicine are funded by private business interests, and may be subject to bias.
Providing objective health-care is becoming more challenging for doctors in all areas of medicine. Private interests can unconsciously influence treatment options that doctors decide to pursue.
A recent study revealed that the United States has one of the highest rates of diagnosed mental disorders of any country in the world. One of the reasons for the high number of diagnoses is bias through private interests.
Pharmaceutical companies manufacturing antidepressants, anxiolytics, and other drugs benefit from a high mental illness diagnosis rate.
5. Liability in Treatment through Online Doctor Reviews
Many doctors are finding themselves screened by patients. There are several prominent websites on the internet that allow patients to review individual doctors, and rate them on their effectiveness.
There have been a number of libel suits against websites offering these review services, but they are becoming a more permanent facet in modern healthcare.
[box type=”important”]Doctors must pay attention to how technology has evolved and changed over the past few decades. For many professionals, continuing education can ensure that doctors and healthcare providers can provide timely and beneficial service to all patients into the future.[/box]
If you want to learn more about how technology and medicine intersect, online universities have specific programs for the same.