Due to the COVID 19 pandemic, healthcare technology – and its importance – has been a real topic of discussion in the last 18 months. The pandemic saw hospitals very nearly overrun at the height of the case toll, which perhaps shined a light on the healthcare technology used and whether it faced up to real scrutiny. Is our healthcare technology efficient enough to scale and treat as many patients as efficiently as possible? This is up for debate – but it has to be said that the NHS did a commendable job given the restraints and very unexpected surge in demand. But how can technology help to make our healthcare service more efficient going forward?

In an ‘Amazon Prime’ world in which we are used to getting services and products ‘on demand’ and ‘next day,’ healthcare must evolve to meet these demands. Generations to come will be even more insistent on convenient healthcare that quickly and conveniently meets their needs. Emerging healthcare technology is contributing to making this expectation a reality.
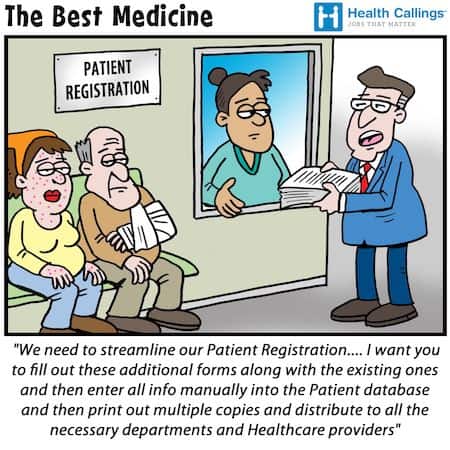
Gone are the days of paper filing and handwritten prescriptions. A new day has dawned with digital versions connected with other organisations across system boundaries. Social and healthcare providers can work together hand in hand, and organisations can share patient records efficiently. Medicines can be safely prescribed and monitored, and a broad skill mix can collaborate on clinical decisions with a shared vision of optimum patient care.
The pandemic may have accelerated the rate in which healthcare technology is being developed. Here we take a look at these examples of health tech in action.
1. Electronic Health Records EHR
Before the deployment of digital patient records, clinical and non-clinical staff had used solely paper records. The introduction of new technological advances ensures all vital information about a patient can be stored in one place, removing the need for paper letters in filing cabinets. The doctor or nurse can quickly flick through digital up to date and rich information, speeding up the process and releasing time to provide better care for the person. The notes can be accessed from a connected laptop or mobile device when away from the base reducing the need to pick up paper notes. Having all the information in front of them enables the care provider to make fully informed and safer decisions.
2. Integrated care
One of the challenges of modern healthcare is how to connect all the different health services that a person might encounter throughout their life.
For example, let’s take a person with dementia and reduced capacity living in a care home with limited family contact. This person will see a mental health specialist both in community and hospital; they may well have other co-morbidities, which might include diabetes, heart failure, respiratory diseases – all of which at some point will need specialist input.
Then, of course, the generalist clinician will be visiting the care home weekly, potentially with another healthcare professional such as a nurse or a pharmacist. Not forgetting the other community care providers- palliative care nurses, advanced clinical nurses for acute incidences, dieticians, dentists, specialist wound nurses, the falls teams.
Every service is individually doing what’s in the patient’s best interest but using separate systems to review backgrounds and talking to the agency staff at the care home to make decisions regarding the person’s care.
By integrating IT systems and patient EHR, there can be more effective partnerships across the health and social care sector with a mix of skills and expertise that provides the best care for the patient in a much more joined-up fashion.
3. Safer use of medicines across the healthcare system
Medications have become part of everyday life for vast numbers of people with multiple health conditions. Clever pharmaceutical experts have and continue to create little parcels of magic that can save a life. But if mishandled, these medicines can be hazardous and can pose a health risk, and it is estimated that between 5-10% of hospital admissions are medicines related.
A clinical practitioner will review all available information before deciding on a medication for a particular diagnosis. This review may include patient preference, medical history, allergies, interactions, and lab data. Some medicines are more high risk and need extra care to ensure effective prescribing and monitoring.
However, time constraints, increasing numbers of patients, and complicated health conditions make this more complex, and occasionally information is missed. Thankfully, specialist technology systems now integrate with the doctors’ software to help with this process and highlight patients that need a clinical medication review or are at high risk of adverse effects through medication.
4. Virtual consultations
Communicating via a phone call is still the norm today, however, health professionals and clinicians must adapt to a virtual world with consultations with patients potentially taking place over the internet. As outlined on the NHS website, a patient can book to consult a doctor anywhere, and digital images can be uploaded and reviewed effectively. And this is all thanks to health tech. Health tech has enabled improved and more convenient access to care services, reducing the inconvenience of travelling, parking, and waiting in line at a GP practice or hospital.
There will always be the need for a person to be reviewed face to face by a healthcare provider. A move to entirely online consultations would be impossible, but tech is making the task of consulting with patients much more convenient.
5. Use of artificial intelligence in hospital departments
Various hospital specialities need medical images such as X-ray, computed tomography CT, and MRI to diagnose and treat disease. As such, radiology is a department that links so closely with all other departments within the hospital.
A radiologist will interpret diagnostic images to help guide diagnosis and the management of the disease. Health tech integration using AI algorithms in radiology has enabled digital versions of images to be organised easily into normal and abnormal within seconds, speeding up the time to diagnosis and, ultimately, treatment.
The radiology department can manage a paperless workflow with mobile devices from around the hospital, and images can be transferred to specialists across geographical borders through teleradiology. So sub-specialist radiologists can be consulted for complex patients around the clock.
Today’s healthcare is finally beginning to meet the modern world’s requirements with these and the many other technological advancements. By working with specialist health tech companies, healthcare organisations can continue to embrace new technologies to help build a strong foundation for further development. It is shaping up to be an exciting future in healthcare.
References
NHS Medicines Value Programme accessed 19.03.21. Available from: https://www.england.nhs.uk/medicines-2/value-programme/
One Comment