Are you having sleepless nights because of your partner snoring? Is your relationship a mess because of the audiological nightmare that you have been experiencing night after night?
While millions of people across the globe suffer from snoring during sleep, the majority are “simple snorers”, also known as primary snorers. There is, however, a segment of snorers (about 100 million people worldwide) that may have a potential health risk.

People who snore, often look like they are in deep slumber and well-rested while keeping you wide awake and terribly disturbed. You expect them to be well-rested and refreshed the next morning after “snoring like a pig”. But often, to your utter surprise and amazement, it is just the opposite. Your partner says, “I had a disturbed sleep last night,” “Hey honey, can I get a strong cup of coffee. I am so, so sleepy,” or “Love, please pass me an Aspirin. My head is aching as if it will explode.”
Before you fire your salvo of expletives at your partner, just remember that your partner’s snoring might be a sign of a more sinister sleep disorder called Obstructive Sleep Apnea (OSA), which is the most common form of sleep-disordered breathing (SDB), a condition of repeated episodes of apnea and hypopnea during sleep.
Beware, snoring, especially obstructive sleep apnea could indicate a deeper health issue in your partner, other than the gripes you are facing in your relationship. Your partner’s life may be at risk!
What is Obstructive Sleep Apnea?
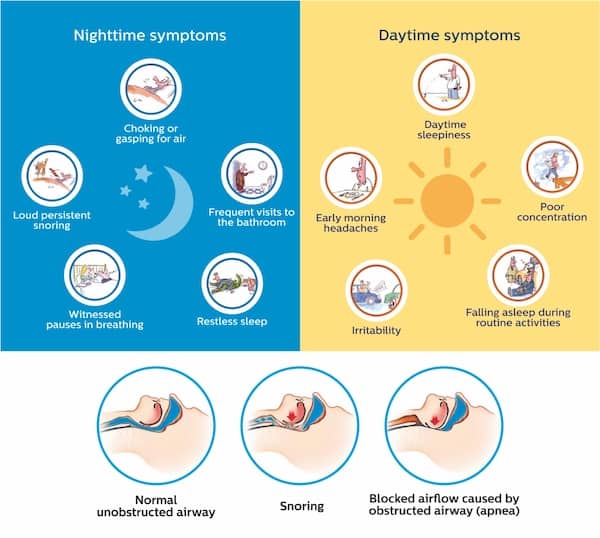
Snoring is caused by vibrating tissues at the back of your mouth and nose, as turbulent airflow occurs through narrowed air passages. This laxity of the muscles and soft tissues at the back of your mouth and nose causes them to fall back on the throat narrowing the upper airway. These lax tissues vibrate with the motions of breathing causing the ghastly “roaring” or “grunting” sound you hear as snoring.
Snoring and sleep-disordered breathing (SDB) are more common among middle-aged men, especially if they are obese with short necks, smoke tobacco, consume alcohol, and are lying supine on their backs. According to a large population-based study by the New England Journal of Medicine, SDBs are seen in 4% of men and 2% of women. Approximately 7–9% of Indian adult population has sleep apnea, higher than those reported from other parts of the world.
Sleep apnea is abnormal, short episodes of breathing pause during sleep. One should have at least five respiratory pauses per hour of sleep to term it as sleep apnea. Obstructive sleep apnea (OSA) is a repetitive, complete or partial obstruction of the upper airway during sleep and causes snoring, reduced oxygen in the body tissues (hypoxia), increased carbon dioxide in the body (hypercapnia) and repeated arousals from sleep.
While most cases of snoring may not be associated with obstructive sleep apnea, it is seen in about 10–25% of snorers. As it occurs due to obstruction of the upper airways, it is commonly known as “Obstructive Sleep Apnea” or OSA. These short breathing pauses or apneas can significantly reduce oxygen supply to the brain and can induce brain injury, in the long run, increasing the risk of heart and neurocognitive impairment.
With the steady rise in the occurrence of obesity and an ageing population, there is bound to be an increase in the number of people who snore and those with Obstructive Sleep Apnea (OSA). Most people with OSA are undiagnosed, untreated or both, leading to a group of people “at-risk” of potentially devastating metabolic and heart diseases.
Should you be worried about your partner snoring?
Yes, you should!
While simple snoring is often harmless, if associated with obstructive sleep apnea (OSA), it may be an early indicator of an incipient systemic ailment. Snoring may be the only signal of impending long-term danger and must be nipped in the bud.
Common long-term consequences of untreated OSA are:
- cardiovascular diseases like uncontrolled hypertension and heart attacks
- metabolic disorders like uncontrolled diabetes and obesity
- cognitive impairment leading to increased risk of motor accidents
- depression with increased risk of suicide
- impotence and failed relationships
Various studies have clinically proven data to prove a significantly high prevalence of sleep apnea in the following medical conditions:
- Drug-resistant Hypertension 80%
- Obesity 77%
- Pacemakers 59%
- Congestive heart failure 50%
- Atrial fibrillation 50%
- Diabetes 50%
- All hypertension 35%
- Coronary artery disease 30%
What this means is that “sleep apnea is commonly found among those with these conditions and not the other way around.”
It is always a good practice to get your partner with a snoring problem evaluated for sleep apnea before ignoring it completely. Sleep interruptions due to snoring and sleep apnea can severely affect a person’s quality of life. Morning headaches, sleepiness during daytime, lethargy and irritability are just a few of the problems that a person with sleep apnea suffers from.
What should you do if your partner has a “big” snoring problem?
If your partner’s snoring has been keeping you awake, or worse still, keeping you both awake and irritated, it is high time you consult with your doctor.
Visiting your doctor is the first step in getting your partner evaluated for sleep apnea and any other dangerous ailments that may be masquerading as snoring.
Diagnosis is the critical first step in the management of Obstructive Sleep Apnea (OSA) as it is a treatable condition.


The following symptoms can indicate that your partner may be having sleep apnea:
- Daytime Symptoms
- Poor concentration
- Daytime sleepiness
- Early morning headaches
- Irritability
- Falling asleep during routine activities
- Nighttime symptoms
- Loud persistent snoring
- Witnessed pauses in breathing
- Choking or gasping for air
- Frequent visits to the bathroom
- Restless sleep
- If your partner has risk factors like obesity, hypertension, stroke history, heart failure, or symptoms such as loud snoring, non-refreshing or disturbed sleep, gasping or choking at night, morning headaches, excessive daytime tiredness and fatigue, he/she should undergo a sleep test to rule out obstructive sleep apnea (OSA).
Is there any tool or app to diagnose obstructive sleep apnea (OSA)?
While a sleep laboratory examination and sleep study is the sure-fire diagnostic method to label someone as having sleep apnea, a simple questionnaire called the “STOP-BANG” Questionnaire can be pretty helpful for screening snorers in the general population.
STOP-BANG is an acronym and represents a set of 8 questions that helps in screening snorers for the risk of obstructive sleep apnea.
- S – Snoring: Do you snore loudly (than talking or loud enough to be heard through closed doors?)
- T – Tired: Do you often feel tired, fatigued or sleepy during daytime?
- O – Observed Apnea: Has anyone observed you stop breathing during your sleep?
- P – Pressure: Do you have or are you being treated for high blood pressure?
- B – BMI: Is your BMI >35 Kg/m2?
- A – Age: Is your age >50 years?
- N – Neck circumference: Is your neck circumference >40 cm?
- G – Gender: Are you male?
There are various mobile and web applications that have integrated the STOP-BANG questionnaire and can easily help you with screening your partner for OSA.
Your partner says “YES” to 3 or more of the STOP-BANG questions.
The first step in the management of possible sleep apnea is a risk assessment using the STOP-BANG questionnaire. This will provide some proof of the existence of an issue.
If your partner answers “YES” to ANY 3 or more of the STOP-BANG questions, he/she may be at high risk of obstructive sleep apnea (OSA) and needs to visit the sleep specialist for an examination and analysis.
Once the risk is assessed by the sleep specialist, the affected person should undergo an overnight sleep test in the clinic or at home.
After analysis and reporting of the sleep study, a customised management plan is chalked out for a person with Obstructive Sleep Apnea (OSA). This involves consideration of the type and severity of sleep-disordered breathing, the patient’s age, gender, BMI, the shape of the head and facial features, co-existing diseases, severity of symptoms and its effect on the quality of life.
This will provide the baseline to start various lifestyle interventions, and if needed, pre-determined therapeutic modalities.
Is there any treatment for snoring and obstructive sleep apnea?
Snoring, without sleep apnea, may be left alone unless it is disturbing the snorer’s quality of life, especially if disturbs a partner’s sleep on a long-term basis. This could adversely affect your relationship causing you to sleep in separate rooms and it can even end up in separation or divorce.
Snoring treatments can vary from simple lifestyle alterations to complex therapeutic modalities, even surgery in some cases. Lifestyle alterations include weight loss, reduction in alcohol consumption, or changing sleeping positions. Some oral devices and nasal strips have been tried to some beneficial effect for those with simple snoring.
Treatment of Obstructive Sleep Apnea, however, is more complex and requires a diagnostic evaluation by a sleep specialist.

The most effective and Gold Standard Treatment for Obstructive Sleep Apnea (OSA) is Continuous Positive Airway Pressure (CPAP). CPAP is a non-invasive treatment where a gentle flow of air is provided directly through the nose and mouth using a mask to prevent the upper airway from collapsing. This allows the subject to breathe more easily by generating positive airway pressure, thus ensuring that adequate oxygen reaches the lungs. This oxygen subsequently reaches blood circulation and ultimately the oxygen-sensitive tissues such as the heart and brain.
While CPAP can be extremely beneficial to the snorer and aids the management of Obstructive Sleep Apnea (OSA), it may feel cumbersome as a CPAP mask has to be worn over the face throughout the night, and has to be tethered to the CPAP machine with a tube. This can be annoying and limiting, especially if you have to be with your partner.
 The DreamStation-AutoCPAP from Philips has a significantly unobtrusive mask with flexible tubing that easily adjusts to various positions of sleep. The intuitive CPAP machine provides automatic breathing support preventing airway closure in every sleeping position and synchronises with the subject’s breathing providing for a restful night for you and your partner as well.
The DreamStation-AutoCPAP from Philips has a significantly unobtrusive mask with flexible tubing that easily adjusts to various positions of sleep. The intuitive CPAP machine provides automatic breathing support preventing airway closure in every sleeping position and synchronises with the subject’s breathing providing for a restful night for you and your partner as well.
DreamMapper is a mobile and web application that integrates with your DreamStation-AutoCPAP and keeps you actively informed about your previous night’s therapy, including your mask fit and therapy hours, ensuring that you get what’s needed for a great night’s sleep.


Philips CPAP devices treat Obstructive Sleep Apnea so that you can sleep better at night and be more active during the day.
Are there any other alternatives to CPAP in treating snoring?
Oral Appliances
An important alternative to CPAP in treating mild to moderate OSA is an oral appliance called Mandibular Advancement Splints (MAS). These appliances are less effective than CPAP but will improve the symptoms to some extent. The good news about oral appliances is that the compliance rate is about 80–90% as compared to 50–70% compliance rate of CPAP. Custom-fitted appliances are more effective compared to the readily available, often poorly-fitting and ineffective over-the-counter models.
Surgery
Surgery of the oropharyngeal soft tissues have been tried with some success, but often, the risks outweigh the benefits. It is useful in a select minority of those affected by OSA.
- Tonsillectomy and adenoidectomy – done when abnormally large tonsils block the upper airway, especially in children.
- Maxillomandibular Advancement Surgery (MMA) with or without genial tubercle advancement – useful in cases with failed treatment with CPAP or MAS. It is a major surgery and carries a much higher risk.
- Multi-level or stepwise surgery (MLS) – this targets correcting multiple levels of upper airway narrowing and has shown improvement in symptoms.
- Laser-assisted uvuloplasty or uvulopalatopharyngoplasty (UPPP) – often fail to relieve symptoms and should not be done as the sole procedure.
- Bariatric surgery – dramatic improvement in symptoms may be noted in severely obese individuals.
- Implantable hypoglossal nerve stimulator – useful in moderate to severe OSA patients who have failed CPAP therapy with good safety and success rate. This treatment is currently approved only in the USA and certain European countries only.
Exercising the oropharyngeal muscles
This is an anecdotally proven way to increase the strength and tone of the soft tissue of the upper airway, thus improving the patency of the upper airway during sleep.
Playing pipe musical instruments is a great example of this technique.
What does recent research suggest about OSA treatment?
Generally speaking, CPAP therapy remains the most effective treatment method for Obstructive Sleep Apnea (OSA) and should be considered by all snorers who manifest symptoms of OSA. CPAP effectively reduces OSA severity and improves cognitive function, sleepiness and blood pressure.
While being compliant to CPAP treatment can reduce the risk of heart ailments in Obstructive Sleep Apnea (OSA) patients, it is not known to show any improvement of heart condition among those already suffering from heart disease and present with only minimal sleepiness.
In Short
If you have been having been suffering long, sleepless nights because of your partner’s snoring, there is hope for you and your partner! You can screen your partner for OSA using the STOP-BANG questionnaire. If your partner is at “high-risk,” take him/her to a Sleep Clinic/Sleep Specialist to get tested for OSA. If OSA is ruining your life and marriage, CPAP will save the day!
#DontSleepOnIt
To know more, visit your nearest doctor today or call on 1800 258 7678.
References:
- Franklin, K. A., & Lindberg, E. (2015). Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. Journal of thoracic disease, 7(8), 1311–1322. https://doi.org/10.3978/j.issn.2072–1439.2015.06.11
- Lee, Y. C., Eun, Y. G., Shin, S. Y., & Kim, S. W. (2013). Prevalence of snoring and high risk of obstructive sleep apnea syndrome in young male soldiers in Korea. Journal of Korean medical science, 28(9), 1373–1377. https://doi.org/10.3346/jkms.2013.28.9.1373
- Al-Jewair, T. S., Nazir, M. A., Al-Masoud, N. N., & Alqahtani, N. D. (2016). Prevalence and risks of habitual snoring and obstructive sleep apnea symptoms in adult dental patients. Saudi medical journal, 37(2), 183–190. https://doi.org/10.15537/smj.2016.2.12852
- Osman, A. M., Carter, S. G., Carberry, J. C., & Eckert, D. J. (2018). Obstructive sleep apnea: current perspectives. Nature and science of sleep, 10, 21–34. https://doi.org/10.2147/NSS.S124657
- Lee CHK, Leow LC, Song PR, Li HH, Ong TH. Acceptance and Adherence to Continuous Positive Airway Pressure Therapy in patients with Obstructive Sleep Apnea (OSA) in a Southeast Asian privately funded healthcare system. Sleep Sci. 2017 Apr-Jun; 10(2): 57–63.
Disclaimer: This article is an awareness initiative of Philips. The readers are advised not to replicate to any information included herein to get any tests done or treat any health problem without consulting a Doctor(s). Philips does not offer medical advice or recommendations and the readers should not rely on the information provided, as a substitute for consultation with Doctor(s). We recommend consulting a Doctor(s), when in doubt or otherwise. The views expressed in the article are the personal opinions of the Doctor(s) and Philips shall not be liable for any damages arising from the contents of this article, including but not limited to direct, indirect, incidental, punitive and consequential damages.